Abstract
Background: Psychosocial stress in patients with cancer has repeatedly been demonstrated to impact long term outcomes including quality of life and mortality. This concept of psychosocial stress is comprised of many different stressors which can impact care and may require specialized intervention. Previous research, primarily conducted in patients with solid tumors, has identified key areas of screening, including evaluation for overall distress, financial concerns, and depressed mood. However, less is known about the impact of these factors on high-risk hematologic malignancies such as acute myeloid leukemia (AML), especially if identified early in the disease course. The primary objective of this study is to determine whether the presence of a positive screen for psychosocial stressors on presentation impacts overall survival (OS) in AML.
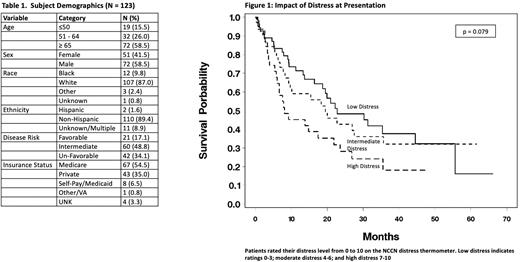
Methods: All patients seen at Levine Cancer Institute, a tertiary hospital-based specialty practice, are asked to complete a tablet based electronic distress screening (EDS) on initial presentation to any specialty clinic. Patients who completed this assessment from 1/1/2017 to 12/31/2021 were then cross-referenced with a clinical AML database maintained by the Leukemia Division. Patients were included for final analysis if they were aged ≥ 18 years, had a verified new diagnosis of AML (excluding acute promyelocytic leukemia), and completed the EDS within 6 months of their diagnosis. Overall distress was assessed using the NCCN Distress thermometer with standard cutoff values (0-3 low, 4-6 moderate, and 7-10 high). Financial concerns were assessed with the question "Do you have insurance/financial problems or concerns?” Depression was assessed with the Patient Health Questionnaire-2 (PHQ-2) with a standard cutoff of score ≥ 3 indicating depressed mood. The primary endpoint was OS, which was calculated as the time from diagnosis until death. For subjects with no death date, OS was censored at the date of last contact. Demographic and disease-specific data were abstracted from the combined databases and electronic medical record review. Baseline demographic and disease characteristics were summarized using descriptive statistics. OS was analyzed by Cox proportional hazards models and Kaplan-Meier techniques. Univariate and multivariate modeling were used to assess the individual and independent prognostic values of overall distress, financial distress, and depressed mood.
Results: A total of 202 patients completed the EDS and had clinical information recorded in the leukemia database for the study period. Of these, 123 patients met criteria for inclusion. Specific characteristics of the analyzed population are listed in Table 1. The population had a median age of 67 years with the majority having ELN 2017 Intermediate (48.8%) or High risk (34.1%) disease. Median time from diagnosis to survey administration was 0.46 months (-3.38 to 5.98 months). Induction strategy was largely hypomethylating agent (HMA)-based, with 43.9% of patient receiving HMA monotherapy or HMA/specific inhibitor and an additional 22.8% of patients receiving HMA/venetoclax. Best response to therapy included 66 patients (53.7%) achieving CR/CRi/CRp, and 51 patients (41.2%) ultimately proceeding to allogeneic hematopoietic stem cell transplantation. Overall distress at presentation was associated with inferior OS, with median OS of 8.1 months for patients reporting high distress, 19.5 months for moderate distress 19.5 months, and 22.8 months for low distress (p = 0.072) (Figure 1). On multivariate modeling, the association between high distress and decreased OS was more pronounced (HR 1.966, 95% CI 1.074-3.598, p = 0.079). There were trends towards decreased OS with endorsement of financial concerns (14.8 vs. 21.0 months) and depressed mood (9.2 vs 19.9 months), but neither trend was found to be statistically significant on uni- and multivariate modeling.
Conclusions: Distress screening early in the disease course for patients with AML identifies a highly vulnerable population with an increased risk of mortality. These patients will likely benefit from early interventions. Financial challenges and depressed mood are also major concerns in the AML population. These findings should be validated in a larger cohort, and early interventional approaches are urgently needed.
Disclosures
Symanowski:Camarus: Consultancy; Eli Lilly & Co.: Consultancy; CARsgen: Consultancy; Immatics: Consultancy. Chojecki:Novartis: Consultancy, Membership on an entity's Board of Directors or advisory committees; Servier: Consultancy, Membership on an entity's Board of Directors or advisory committees; Incyte: Research Funding. Walsh:Helsinn: Consultancy, Other: Unpaid consultancy. Grunwald:AbbVie, Agios/Servier, Amgen, Astellas Pharma, Blueprint Medicines, Bristol Myers Squibb, Cardinal Health, CTI BioPharma, Daiichi Sankyo, Gamida Cell, Gilead Sciences, Incyte Corporation, Invitae, Karius, Novartis, Ono Pharmaceuticals, Pfizer, ,: Consultancy; Genetech/Roche, Incyte Corporation, Janssen: Research Funding; Medtronic: Current equity holder in private company; Daiichi Sankyo, Gamida Cell, Gilead Sciences, Incyte Corporation, Invitae, Karius, Novartis, Ono Pharmaceutical, Pfizer, Pharmacosmos, Premier, Sierra Oncology, Stemline Therapeutics: Consultancy.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal